Your Body, Your Choice: How Many Embryos to Transfer?
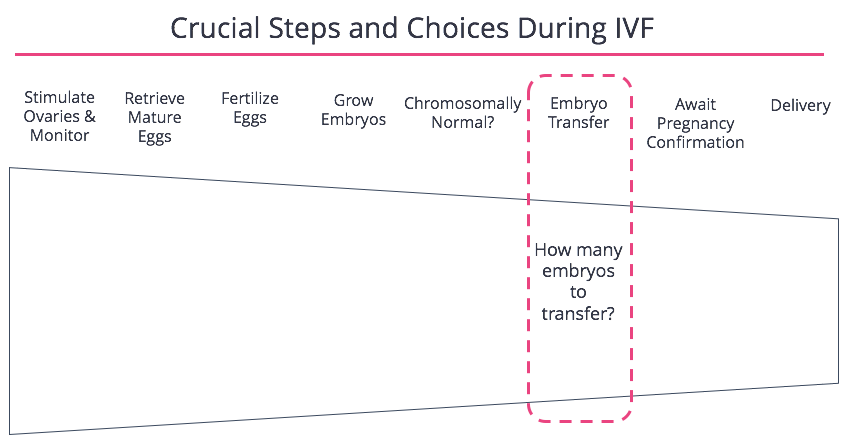
The decision to embark on in-vitro fertilization (IVF) is often a deeply personal one, fraught with hope, expectation, and a multitude of complex choices. Among the most significant of these is the question of how many embryos to transfer. This seemingly simple decision, framed by the powerful phrase “Your Body, Your Choice,” carries profound implications for the success of the IVF cycle, the health of the mother, and the well-being of any resulting children. Understanding the factors involved in this critical choice is paramount, requiring a careful balancing act between the desire for a successful pregnancy and the potential risks associated with multiple gestations. This article will delve into the intricacies of embryo transfer, providing a comprehensive overview of the considerations involved, empowering individuals to make informed decisions that align with their personal circumstances and values. The core principle of “Your Body, Your Choice” underscores the importance of patient autonomy in this process.
The Evolution of Embryo Transfer Practices
The landscape of IVF has dramatically evolved since its inception. Early IVF cycles often involved transferring multiple embryos to increase the chances of a successful pregnancy. However, this practice resulted in a significantly higher rate of multiple births, including twins, triplets, and even higher-order multiples. While multiple births can be joyous occasions, they also carry significant risks, including preterm labor, low birth weight, gestational diabetes, preeclampsia, and an increased likelihood of cesarean delivery for the mother. For the babies, multiple births are linked to increased rates of cerebral palsy, developmental delays, and other health complications. Recognizing these risks, medical professionals and patient advocacy groups have worked to refine embryo transfer protocols. The shift has been towards a more cautious approach, with a growing emphasis on single embryo transfer (SET) whenever possible. This shift reflects a commitment to improving outcomes for both the mother and the child(ren), prioritizing the health and safety of all involved. The principle of “Your Body, Your Choice” remains central to this, as the patient ultimately makes the final decision in consultation with their medical team.
Factors Influencing the Decision
The decision of how many embryos to transfer is not a one-size-fits-all scenario. Several factors must be carefully considered, including:
- Patient Age: A woman’s age is a crucial factor. Younger women, with higher-quality embryos, may have a greater chance of success with SET. Older women, who may have fewer high-quality embryos, might be advised to transfer more embryos to increase the likelihood of pregnancy.
- Embryo Quality: The quality of the embryos, assessed through microscopic evaluation, is a key determinant. Embryos graded as high-quality have a better chance of implanting and developing into a healthy fetus.
- Previous IVF History: A woman’s prior IVF experience, including any previous successes or failures, helps guide decision-making.
- Number of Embryos Available: The number of viable embryos available for transfer is a practical consideration.
- Patient Preferences and Values: The patient’s personal preferences and values are paramount. Some individuals may be more comfortable with the possibility of multiple births, while others prioritize the health and safety of a singleton pregnancy. The phrase “Your Body, Your Choice” is particularly relevant here.
- Clinic Policies: Different IVF clinics have varying policies regarding embryo transfer, often influenced by their success rates, ethical considerations, and local regulations.
These factors are carefully weighed by the patient and their medical team, leading to a personalized treatment plan. It’s crucial to have open and honest communication with your doctor, discussing your concerns, priorities, and any questions you may have. The ultimate goal is to find the optimal balance between maximizing the chances of a successful pregnancy and minimizing potential risks. “Your Body, Your Choice” highlights the patient’s central role in this process.
Single Embryo Transfer (SET) – The Preferred Approach?
As mentioned earlier, SET is increasingly becoming the preferred approach, especially for younger patients with high-quality embryos. The benefits of SET are clear: significantly reduced risk of multiple gestations and the associated complications. While SET might result in a slightly lower chance of pregnancy per cycle compared to transferring multiple embryos, the improved outcomes for both mother and child often make it the most desirable option. However, SET is not always feasible or appropriate. For some patients, particularly those with advanced maternal age or a history of failed IVF cycles, transferring multiple embryos may be considered to increase the chances of pregnancy. The decision is always made on a case-by-case basis, taking into account the individual’s specific circumstances. The concept of “Your Body, Your Choice” allows for this flexibility, recognizing that what is best for one person may not be best for another.
The Role of Preimplantation Genetic Testing (PGT)
PGT is a sophisticated technology that allows for the genetic screening of embryos before transfer. This testing can identify embryos with chromosomal abnormalities, which are a leading cause of implantation failure and miscarriage. PGT can also be used to screen for specific genetic disorders. By selecting genetically healthy embryos for transfer, PGT can improve the chances of a successful pregnancy and reduce the risk of complications. PGT can also play a role in determining how many embryos to transfer. If a patient has multiple genetically healthy embryos, SET may be a viable option. If only a few embryos are deemed genetically healthy, transferring more than one embryo may be considered. The use of PGT further enhances the ability to personalize the embryo transfer process, aligning with the principle of “Your Body, Your Choice” by providing more information and control to the patient.
The Ethical and Emotional Considerations
The decision of how many embryos to transfer extends beyond medical considerations and involves significant ethical and emotional dimensions. For many individuals, the prospect of multiple births can be emotionally challenging, raising concerns about their ability to provide adequate care and support for multiple children. There are also complex ethical considerations, such as the potential for selective reduction (reducing the number of fetuses in a multiple pregnancy), which is a difficult and emotionally charged decision. Furthermore, the disposal of unused embryos raises ethical questions for some individuals. It is essential to have open discussions with your medical team, family, and support system to address these concerns. Counseling and support groups can provide valuable emotional support during this challenging process. Remembering “Your Body, Your Choice” means acknowledging and respecting the emotional journey.
Making an Informed Decision: A Step-by-Step Guide
Making the right decision about embryo transfer requires a proactive and informed approach. Here is a step-by-step guide:
- Consultation with a Fertility Specialist: The first step is to consult with a qualified fertility specialist. Discuss your medical history, reproductive goals, and any concerns you may have.
- Comprehensive Evaluation: Undergo a thorough evaluation, including blood tests, ultrasound scans, and a review of your partner’s sperm analysis (if applicable).
- Embryo Quality Assessment: Understand how your embryos are graded and what those grades mean in terms of their potential for implantation.
- Review of Clinic Policies: Familiarize yourself with the clinic’s policies regarding embryo transfer, including their success rates and their approach to SET.
- Discussion of Risks and Benefits: Have a detailed discussion with your doctor about the risks and benefits of transferring one or more embryos.
- Consider PGT: Discuss the potential benefits of PGT and whether it is appropriate for your situation.
- Explore Your Values and Preferences: Reflect on your personal values, priorities, and comfort level with the possibility of multiple births. The phrase “Your Body, Your Choice” is a reminder to center your preferences.
- Seek Emotional Support: Consider counseling or support groups to help you navigate the emotional aspects of IVF.
- Make an Informed Decision: Based on all the information gathered, work with your doctor to make an informed decision that aligns with your goals and values.
- Celebrate Your Choice: Remember, whatever decision you make is the right one for you. Embrace your choice and celebrate your journey.
This process empowers you to make a decision that reflects “Your Body, Your Choice.”
The Future of Embryo Transfer
The field of reproductive medicine is constantly evolving. Research continues to refine embryo selection techniques and improve outcomes. Advances in PGT, including non-invasive methods, are promising. Furthermore, research on endometrial receptivity (the ability of the uterine lining to accept an embryo) is leading to a more personalized approach to embryo transfer. These advancements will further empower patients to make informed decisions that align with their individual needs and preferences, solidifying the principle of “Your Body, Your Choice.” The future holds even greater opportunities for optimizing the IVF process and achieving successful and healthy pregnancies. “Your Body, Your Choice” will continue to shape the conversation.
Conclusion: Embracing the Power of Choice
The decision of how many embryos to transfer is a pivotal one in the IVF journey. It is a decision that demands careful consideration, open communication, and a deep understanding of the medical, ethical, and emotional factors involved. By embracing the principle of “Your Body, Your Choice,” individuals can take control of their reproductive health and make informed decisions that align with their personal values and goals. The advancements in reproductive medicine, coupled with a commitment to patient-centered care, are paving the way for a brighter future for those seeking to build their families. Ultimately, the power lies in the hands of the individual, guided by the expertise of medical professionals and supported by a network of care. This journey is about “Your Body, Your Choice.”
[See also: Related Article Titles]

